Measles Outbreak
https://www.cnn.com/2019/01/26/health/washington-state-measles-state-of-emergency/index.html
(CNN)As of Sunday, there are 35 confirmed cases of measles in the state of Washington -- an outbreak that has already prompted Gov. Jay Inslee to declare a state of emergency.
Most patients with symptoms should call first
TB Blood Test
TB Blood Tests
What is an Interferon Gamma Release
Assay (IGRA)?
An IGRA is a blood test that can determine if a person has been infected with TB bacteria. An IGRA measures how strong a person’s immune system reacts to TB bacteria by testing the person’s blood in a laboratory.Two IGRAs are approved by the U.S. Food and Drug Administration (FDA) and are available in the United States:
1) QuantiFERON®-TB Gold In-Tube test
(QFT-GIT)
2) T-SPOT®.TB test (T-Spot)
How does the IGRA work?
Blood is collected into special tubes using a needle. The blood is delivered to a laboratory as directed by the IGRA test instructions. The laboratory runs the test and reports the results to the health care provider.
What does a positive IGRA result mean?
Positive IGRA: This means that the person has been infected with TB bacteria. Additional tests are needed to determine if the person has latent TB infection or TB disease. A health care worker will then provide treatment as needed.
Negative IGRA: This means that the person’s blood did not react to the test and that latent TB infection or TB disease is not likely.
Who can receive an IGRA?
Anyone can have an IGRA in place of a TST. This canbe for any situation where a TST is recommended. In general, a person should have either a TST or an IGRA, but not both. There are rare exceptions when results from both tests may be useful in deciding whether a
person has been infected with TB.
IGRAs are the preferred method of TB infection testing
for the following:
- People who have received the BCG shot
- People who have a difficult time returning for a
second appointment to look at the TST after the test was given
How often can an IGRA be given?
There is no problem with repeated IGRAs. Who Should Get Tested for TB?
Certain people should be tested for TB bacteria because they are more likely to get TB disease, including:
- People who have spent time with someone who has TB disease
- People with HIV infection or another medical problemthat weakens the immune system
- People who have symptoms of TB disease (fever, night sweats, cough, and weight loss)
- People from a country where TB disease is common (most countries in Latin America, the Caribbean, Africa, Asia, Eastern Europe, and Russia)
- People who live or work somewhere in the United States where TB disease is more common (homeless shelters, prison or jails, or some nursing homes)
- People who use illegal drugs
When Should You Suspect Tuberculosis (TB)?
TB is a disease caused by Mycobacterium
tuberculosis. TB disease should be suspected in persons who have the following symptoms:
- Unexplained weight loss
- Loss of appetite
- Night sweats
- Fever
- Fatigue
If TB disease is in the lungs (pulmonary), symptoms may include:
- Coughing for ≥3 weeks
- Hemoptysis (coughing up blood)
- Chest pain
If TB disease is in other parts of the body (extrapulmonary), symptoms will depend on the area affected.

How Do You Evaluate Persons Suspected of Having TB Disease?
A complete medical evaluation for TB includes the following:
-
Medical History
Clinicians should ask about the patient’s history of TB exposure, infection, or disease.
It is also important to consider demographic factors (e.g., country of origin, age, ethnic or racial group, occupation) that may increase the patient’s risk for exposure to TB or to drug resistantAlso, clinicians should determine whether the patient has medical conditions, especially HIV infection, that increase the risk of latent TB infection progressing to TB disease.
-
. Physical Examination
A physical exam can provide valuable information about the patient’s overall
condition and other factors that may affect how TB is treated, such as HIV infection or other illnesses.
-
Test for TB Infection
The Mantoux tuberculin skin test (TST) or the TB blood test can be used to test for M. tuberculosis infection. Additional tests are required to confirm TB disease. The Mantoux tuberculin skin test is performed by injecting a small amount of fluid called tuberculin into the skin in the lower part of the arm. The test is read within 48 to 72 hours by a trained
health care worker, who looks for a reaction (induration) on the arm. -
Chest Radiograph
A posterior-anterior chest radiograph is used to detect chest abnormalities. Lesions may appear anywhere in the lungs and may differ
in size, shape, density, and cavitation. These abnormalities may suggest TB, but cannot be used to definitively diagnose TB. However, a
chest radiograph may be used to rule out the possibility of pulmonary TB in a person who has had a positive reaction to a TST or TB blood
test and no symptoms of disease. -
Diagnostic Microbiology
The presence of acid-fast-bacilli (AFB) on a sputum smear or other specimen often indicates TB disease. Acid-fast microscopy is easy and quick, but it does not confirm a diagnosis of TB because some acid-fast-bacilli are not M. tuberculosis. Therefore, a culture is done on all initial samples to confirm the diagnosis. (However, a positive culture
is not always necessary to begin or culture for M. tuberculosis confirms
the diagnosis of TB disease. Culture examinations should be completed on all specimens, regardless of AFB smear results. Laboratories should report positive results on smears and cultures within 24 hours by telephone or fax to the primary health care provider and to
the state or local TB control program, as required by law. -
Drug Resistance
For all patients, the initial M. tuberculosis isolate should be tested for drug resistance. It is crucial to identify drug resistance as early as possible to ensure effective treatment. Drug susceptibility patterns should be repeated for patients.
2 step TB test
Baseline Testing: Two-Step Test
Two-step testing with the Mantoux tuberculin skin test (TST) should be used for baseline or initial testing. Some people with latent TB infection have a negative reaction when tested years after being infected. The first TST may stimulate or boost a reaction. Positive reactions to subsequent TSTs could be misinterpreted as a recent infection.
Step 1
- Administer first TST following proper protocol
- Review result
- Positive — consider TB infected, no second TST needed; evaluate for TB disease.
- Negative — a second TST is needed. Retest in 1–3 weeks after first TST result is read.
- Document result
Step 2
- Administer second TST 1-3 weeks after first test
- Review results
- Positive — consider TB infected and evaluate for TB disease.
- Negative — consider person not infected.
- Document result
Two-Step TST Testing

Blood Test vs Skin Test…
If you are going to struggle to go back for a follow up appointment for the TST then the blood test will be best as only one test is required and the results are given electronically.
False positives can occur in a TST if you have had a BCG.
What is Tuberculosis and what are symptom
What is tuberculosis?
Tuberculosis (TB) is a disease caused by infection with bacteria called Mycobacterium tuberculosis. TB usually affects the lungs (respiratory infection), but it can affect other parts ofthe body as well.
When a person who has a respiratory TB infection coughs, sneezes, or spits, droplets containing TB bacteria are released into the air. If another person breathes
in those droplets, he or she becomes exposed to the bacteria. This is how TB bacteria are typically spread from one person to another.
Not everyone who has TB bacteria in their bodies will become sick. Those who do not become sick are said to have latent TB infection. Those who do become sick have an active infection.
• People with latentTB infections usually have strong natural defense (immune) systems that keep the
TB bacteria from multiplying. They do not develop TB symptoms and cannot spread TB to others. It is
possible, however,for a person with a latent infection
to develop an active infection. This happens to about 1 in 10 people who have untreated latent TBinfections.1
• An active TB infection means the TB bacteria
are multiplying. This will cause a person to have symptoms ofTB disease. Active TB is highly contagious (easily spread from one person
to another) .
Certain people are at greater risk of developing an active TB infection when exposed to TB bacteria. These include people who1-3:
• Have recently (within the past 2 years) been infected with TB bacteria.
• Were not correctly treated forTB infection in the past.
• Have medical conditions (such as pregnancy, HIV infection,diabetes,or cancer) or take medications (such as those used to prevent rejection after an organ transplant) that weaken the immune system.
• Live in (or recently relocated from) parts of the world where the rates ofTB infection are high.
• Are in close contact (either at work , school, or home) with 1 or more people who have an active TB infection.
• Smoke.
• Abuse alcohol or drugs.
Symptoms of an active TB infection may include1.3:
• A long-lasting cough that may bring up bloody mucus (sputum) .
• Chest pains.
• Unexplained weight loss.
• Loss of appetite.
• Weakness or tiredness (fatigue).
• Fever.
• Night sweats.
Without treatment, an active TB infection may cause serious illness or even death. TB is treated with a combination of antibiotics that must be taken for several months.

Thyroid Testing
It is estimated that 20 million Americans have some form of thyroid disease.
New studies show that 13 million Americans may be either unaware of or undiagnosed with a thyroid condition and that more widespread thyroid testing is needed. Undiagnosed thyroid disease may put us at risk for certain serious medical conditions, such as cardiovascular diseases, osteoporosis and infertility. Anyone can develop a thyroid disorder - even babies. However, women are five to eight times more likely than men to have thyroid problems. One woman in eight will develop a thyroid disorder during her lifetime.
There are several different thyroid disorders, but two of the most common are hypothyroidism (underactive thyroid) and hyperthyroidism (overactive thyroid).
Why Get Tested?
To help evaluate thyroid gland function and to help diagnose thyroid disorders
When to Get Tested?
When you have signs and symptoms suggesting hypo- or hyperthyroidism due to a condition affecting the thyroid
How is the Thyroid Panel Used?
A thyroid panel is used to evaluate thyroid function and/or help diagnose hypothyroidism and hyperthyroidism due to various thyroid disorders. The panel typically includes tests for:
- Thyroid-stimulating hormone (TSH)
- Free thyroxine (free T4)
- Total or free triiodothyronine (total or free T3)
T4 and T3 are hormones produced by the thyroid gland. They help control the rate at which the body uses energy, and are regulated by a feedback system. TSH from the pituitary gland stimulates the production and release of T4 (primarily) and T3 by the thyroid. Most of the T4 and T3 circulate in the blood bound to protein. A small percentage is free (not bound) and is the biologically active form of the hormones.
Laboratory tests can measure either total amount of hormone (bound plus unbound) or just the free portion. The free T4 test is thought by many to be a more accurate reflection of thyroid hormone function and, in most cases, its use has replaced that of the total T4 test. However, some professional guidelines still recommend the total T3 test so either free T3 or total T3 may be ordered by a health practitioner.
Typically, the preferred initial test for thyroid disorders is a TSH test. If the TSH level is abnormal, it will usually be followed up with a test for free T4. Sometimes a total T3 or free T3 will also be performed. Often, the laboratory will do this follow-up testing automatically. This is known as reflex testing and it saves the health practitioner time from having to wait for the results of the initial test and then requesting additional testing to confirm or clarify a diagnosis. Reflex tests are typically performed on the original sample that was submitted when the initial test was requested.
As an alternative, a thyroid panel may be requested by the health practitioner. This means that all three tests will be performed at the same time to get a more complete initial picture of thyroid function.
When is it ordered?
A thyroid panel may be ordered when symptoms suggest hypo- or hyperthyroidism due to a condition affecting the thyroid.
Signs and symptoms of hypothyroidism may include:
- Weight gain
- Dry skin
- Constipation
- Cold intolerance
- Puffy skin
- Hair loss
- Fatigue
- Menstrual irregularity in women
Signs and symptoms of hyperthyroidism may include:
- Increased heart rate
- Anxiety
- Weight loss
- Difficulty sleeping
- Tremors in the hands
- Weakness
- Diarrhea
- Puffiness around the eyes, dryness, irritation, or bulging of the eyes
What does the thyroid results mean?
If the feedback system involving the thyroid gland is not functioning properly due to one of a variety of disorders, then increased or decreased amounts of thyroid hormones may result. When TSH concentrations are increased, the thyroid will make and release inappropriate amounts of T4 and T3 and the person may experience symptoms associated with hyperthyroidism. If there is decreased production of thyroid hormones, the person may experience symptoms of hypothyroidism.
The following table summarizes some examples of typical test results and their potential meaning.
| TSH | T4 | T3 | Interpretation |
|---|---|---|---|
| High | Normal | Normal | Mild (subclinical) hypothyroidism |
| High | Low | Low or normal | Hypothyroidism |
| Low | Normal | Normal | Mild (subclinical) hyperthyroidism |
| Low | High or normal | High or normal | Hyperthyroidism |
| Low | Low or normal | Low or normal | Nonthyroidal illness; pituitary (secondary) hypothyroidism |
| Normal | High | High | Thyroid hormone resistance syndrome (a mutation in the thyroid hormone receptor decreases thyroid hormone function) |
The above test results alone are not diagnostic but will prompt a health practitioner to perform additional testing to investigate the cause of the excess or deficiency and thyroid disorder. As examples, the most common cause of hyperthyroidism is Graves disease and the most common cause of hypothyroidism is Hashimoto thyroiditis. (See the condition article on Thyroid Diseases for more on these and other related diseases.)
Is there anything else I should know?
In the past, panels of tests were more common. More recently, however, the practice has been to order, where possible, one initial or screening test and then follow up with additional testing, if needed, to reduce the number of unnecessary tests. With thyroid testing, one strategy is to screen with a TSH test and then order additional tests if the results are abnormal or if clinical suspicions warrant.
It is important to note that thyroid tests are a "snapshot" of what is occurring within a dynamic system. An individual person's total T4, free T4, total T3, free T3, and/or TSH results may vary and may be affected by:
- Increases, decreases, and changes (inherited or acquired) in the proteins that bind T4 and T3
- Pregnancy
- Estrogen and other drugs
- Liver disease
- Systemic illness
- Resistance to thyroid hormones
- Pituitary dysfunction
Hypothyroidism
- Extreme tiredness or lethargy
- Memory Loss
- Depression or mood swings
- Constipation
- Weight Gain
- 3 pm Crash
- Broken Sleep
- Brittle or Ridged Nails
- Joint/muscle pain
- Swelling of the face
- Hoarseness
- Slow heart rate
- Feeling cold when others are comfortable
- Hair loss
- Dry skin
Hyperthyroidism
- Bulging of the Eyes
- Breathlessness
- Nervousness
- Trouble concentrating
- Difficulty sleeping
- Insomnia
- Fast heart rate
- Diarrhea
- Heart palpitations
- Weakness
- Hair loss
- Staring Gaze
- Nausea and vomiting
- Warm moist skin
- Trembling hands
- Weight loss without trying
What is being tested?
A thyroid panel is a group of tests that may be ordered together to help evaluate thyroid gland function and to help diagnose thyroid disorders. The tests included in a thyroid panel measure the amount of thyroid hormones in the blood. These hormones are chemical substances that travel through the blood and control or regulate the body's metabolism–how it functions and uses energy.
The thyroid panel usually includes:
- TSH (thyroid-stimulating hormone) - to test for hypothyroidism, hyperthyroidism and to monitor treatment for a thyroid disorder
- Free T4 (thyroxine) - to test for hypothyroidism and hyperthyroidism; may also be used to monitor treatment
- Free T3 or total T3 (triiodothyronine) - to test for hyperthyroidism; may also be used to monitor treatment
Sometimes a T3 resin uptake (T3RU) test is included to calculate, along with the T4 value, the free thyroxine index (FTI), another method for evaluating thyroid function that corrects for changes in certain proteins that can affect total T4 levels.

TSH is produced by the pituitary gland and is part of the body's feedback system to maintain stable amounts of the thyroid hormones T4 and T3 in the blood. When thyroid hormone levels decrease, the pituitary is stimulated to release TSH. TSH in turn stimulates the production and release of T4 and T3 by the thyroid gland. When the system is functioning normally, thyroid production turns on and off to maintain constant blood thyroid hormone levels.
T3 and T4 are the two major hormones produced by the thyroid gland, a small butterfly-shaped organ that lies flat across the windpipe at the base of the throat. Together they help control the rate at which the body uses energy. Almost all of the T3 and T4 circulating in the blood is bound to protein. The small portions that are not bound or "free" are the biologically active forms of the hormones. Tests can measure the amount of free T3 or free T4 or the total T3 or total T4 (bound plus unbound) in the blood.
The total T4 and total T3 tests have been used for many years, but they can be affected by the amount of protein available in the blood to bind to the hormone. The free T4 and free T3 tests are not affected by protein levels and are thought by many to be more accurate reflections of thyroid hormone function. In most cases, the free T4 test has replaced that of the total T4 test. However, some professional guidelines recommend the total T3 test, so either total T3 or free T3 test may be used to assess thyroid function.
What conditions are associated with hypo- and hyperthyroidism?
The most common causes of thyroid dysfunction are autoimmune-related. Graves disease causes hyperthyroidism and Hashimoto thyroiditis causes hypothyroidism. Both hyper- and hypothyroidism can also be caused by thyroiditis, thyroid cancer, and excessive or deficient production of TSH
What other tests may be ordered in addition to a thyroid panel?
Blood tests that may be performed in addition to a thyroid panel may include:
-
- Thyroid Antibodies - to help differentiate different types of thyroiditis and identify autoimmune thyroid conditions
- Calcitonin - to help detect the presence of excessive calcitonin production as can occur with C-cell hyperplasia and medullary thyroid cancer
- Thyroglobulin - to monitor treatment of thyroid cancer
- Thyroxine-binding globulin (TBG) - to evaluate patients with abnormal T4 and T3 levels
-
What is reverse T3?
Reverse T3 (RT3 or REVT3) is a biologically inactive form of T3. Normally, when T4 is converted to T3 in the body, a certain percentage of the T3 is in the form of RT3. When the body is under stress, such as during a serious illness, thyroid hormone levels may be outside of normal ranges even though there is no thyroid disease present. RT3 may be elevated in non-thyroidal conditions, particularly the stress of illness. It is generally recommended that thyroid testing be avoided in hospitalized patients or deferred until after a person has recovered from an acute illness. Use of the RT3 test remains controversial, and it is not widely requested.

TB Blood Testing
What is a TB blood test?
The tuberculosis (TB) blood test, also called an Interferon Gamma Release Assay or IGRA, is a way to find out if you have TB germs in your body. The TB blood test can be done instead of a TB skin test (Mantoux). There are two kinds of TB blood tests: • QuantiFERON®-TB • T-SPOT®.
TB You should have a TB blood (or TB skin test) if you:
- have had frequent close contact with someone who has active TB disease,
- have lived in a country where many people have TB
- work or live in a nursing home, clinic, hospital, prison, or homeless shelter, or
- have HIV infection or your immune system is not very strong.
- Children less than 5 years old should have the TB skin test instead of the TB blood test. How can I get a TB blood test?
What if my TB blood is “negative”?
A “negative” TB blood test result usually means that you don’t have TB germs in your body.
What if my TB blood is “positive”?
A “positive” TB blood test result means you probably have TB germs in your body. Most people with a positive TB blood test have latent TB infection. To be sure, you will need to do a chest x-ray.
You may need other tests to see if you have latent TB infection or active TB disease. What is latent TB infection? There are two phases of TB. Both phases can be treated with medicine. When TB germs enter your body, they cause latent TB infection. Without treatment, latent TB infection can become active TB disease.
What if I’ve had the BCG vaccine?
The BCG vaccine (TB vaccine) may help protect young
children from getting very sick with TB. This protection goes away as people get older.
People who have had BCG vaccine still can get latent TB infection and active TB disease.
If you had the BCG vaccine and you have a choice of having a TB blood test or a TB skin test, it is better for you to have the TB blood test. This is because the TB blood test is not affected by the BCG vaccine. This means that your TB blood test will be “positive” only if you have TB germs in your body.
Protect your health and the health of your family – get a TB blood test!

TB Blood Testing alternative to TB Skin test
TB blood tests are the preferred TB test for:
- People who have received the TB vaccine bacille Calmette–Guérin (BCG). TB blood tests (IGRAs), unlike the TB skin test, are not affected by prior BCG vaccination and are not expected to give a false-positive result in people who have received BCG. TB blood tests are the preferred method of TB testing for people who have received the BCG vaccine.
- People who have a difficult time returning for a second appointment to look for a reaction to the TST.
TB blood tests are also called interferon-gamma release assays or IGRAs. Two TB blood tests are approved by the U.S. Food and Drug Administration (FDA) and are available in the United States: the QuantiFERON®–TB Gold In-Tube test (QFT-GIT) and the T-SPOT®.TB test (T-Spot).
A health care provider will draw a patient’s blood and send it to a laboratory for analysis and results.
- Positive TB blood test: This means that the person has been infected with TB bacteria. Additional tests are needed to determine if the person has latent TB infection or TB disease.
- Negative TB blood test: This means that the person’s blood did not react to the test and that latent TB infection or TB disease is not likely.
TB Blood tests
Blood tests may be used to confirm or rule out latent or active tuberculosis. These tests use sophisticated technology to measure your immune system's reaction to TB bacteria. QuantiFERON-TB Gold in-Tube test and T-Spot.TB test are two examples of TB blood tests.
These tests require only one office visit. A blood test may be useful if you're at high risk of TB infection but have a negative response to the skin test, or if you've recently received the BCG vaccine.
Imaging tests
If you've had a positive skin test, your doctor is likely to order a chest X-ray or a CT scan. This may show white spots in your lungs where your immune system has walled off TB bacteria, or it may reveal changes in your lungs caused by active tuberculosis. CT scans provide more-detailed images than do X-rays.
What is Hep B and how effective is vaccination.
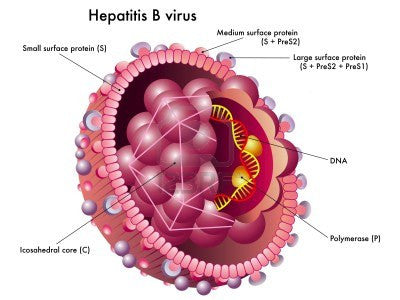
What is Hepatitis B?
Hepatitis B is an infection caused by the hepatitis B virus (HBV), which is transmitted through percutaneous (i.e., breaks in the skin) or mucosal (i.e., direct contact with mucous membranes) exposure to infectious blood or body fluids. The virus is highly infectious; for nonimmune persons, disease transmission from a needlestick exposure is up to 100 times more likely for exposure to hepatitis B e antigen (HBeAg)--positive blood than to HIV-positive blood (14).
HBV infection is a well recognized occupational risk for U.S. HCP and globally. The risk for HBV is associated with degree of contact with blood in the work place and with the hepatitis B e-antigen status of the source persons (15). The virus is also environmentally stable, remaining infectious on environmental surfaces for at least 7 days (16).
In 2009 in the United States, 3,371 cases of acute HBV infection were reported nationally, and an estimated 38,000 new cases of HBV infection occurred after accounting for underreporting and underdiagnosis (17). Of 4,519 persons reported with acute HBV infection in 2007, approximately 40% were hospitalized and 1.5% died (18). HBV can lead to chronic infection, which can result in cirrhosis of the liver, liver failure, liver cancer, and death.
An estimated 800,000--1.4 million persons in the United States are living with chronic HBV infection; these persons serve as the main reservoir for continued HBV transmission (19).
Hepatitis B Vaccine Info
Vaccines to prevent hepatitis B became available in the United States in 1981; a decade later, a national strategy to eliminate HBV infection was implemented, and the routine vaccination of children was recommended (20). During 1990--2009, the rate of new HBV infections declined approximately 84%, from 8.5 to 1.1 cases per 100,000 population (17); the decline was greatest (98%) among persons aged <19 years, for whom recommendations for routine infant and adolescent vaccination have been applied. Although hepatitis B vaccine coverage is high in infants, children, and adolescents (91.8% in infants aged 19--35 months and 91.6% in adolescents aged 13--17 years) (21,22), coverage remains lower (41.8% in 2009) for certain adult populations, including those with behavioral risks for HBV infection (e.g., men who have sex with men and persons who use injection drugs) (23).
How Effective is the Hepatitis B Vaccine?
The 3-dose vaccine series administered intramuscularly at 0, 1, and 6 months produces a protective antibody response in approximately 30%--55% of healthy adults aged ≤40 years after the first dose, 75% after the second dose, and >90% after the third dose (40--42). After age 40 years, <90% of persons vaccinated with 3 doses have a protective antibody response, and by age 60 years, protective levels of antibody develop in approximately 75% of vaccinated persons (43). Smoking, obesity, genetic factors, and immune suppression also are associated with diminished immune response to hepatitis B vaccination (43--46).
How long with immunity last after Vaccination?
Protection against symptomatic and chronic HBV infection has been documented to persist for ≥22 years in vaccine responders.
Hepatitis B for Healthcare employees
During 1982, when hepatitis B vaccine was first recommended for HCP, an estimated 10,000 infections occurred among persons employed in a medical or dental field. By 2004, the number of HBV infections among HCP had decreased to an estimated 304 infections, largely resulting from the implementation of routine preexposure vaccination and improved infection-control precautions (24--26).
The risk for acquiring HBV infection from occupational exposures is dependent on the frequency of percutaneous and mucosal exposures to blood or body fluids (e.g., semen, saliva, and wound exudates) containing HBV, particularly fluids containing HBeAg (a marker for high HBV replication and viral load) (27--31). The risk is higher during the professional training period and can vary throughout a person's career (1). Depending on the tasks performed, health-care or public safety personnel might be at risk for HBV exposure; in addition, personnel providing care and assistance to persons in outpatient settings and those residing in long-term--care facilities (e.g., assisted living) might be at risk for acquiring or facilitating transmission of HBV infection when they perform procedures that expose them to blood (e.g., assisted blood-glucose monitoring and wound care)
Other Considerations
Occupational health programs and others responsible for infection prevention and control should identify all staff whose work-related activities involve exposure to blood or other potentially infectious body fluids in a health-care, laboratory, public safety, or institutional setting (including employees, students, contractors, attending clinicians, emergency medical technicians, paramedics, and volunteers); provide education to staff to encourage vaccination; and implement active follow-up, with reminders to track completion of the vaccine series and postvaccination testing among persons receiving vaccination (72).
In partnership with state and local health authorities, household, sex, or needle-sharing contacts of HBsAg-positive HCP and trainees should be identified, tested, vaccinated (if indicated), and provided with counseling and referral for needed services, when appropriate.
Information from CDC
Hep B Transmission
Hepatitis B is found in blood and in body fluids, including semen and vaginal fluids. Even though studies have shown minute quantities of the virus can be present in saliva, tears and breast milk, they are not considered to be in high enough levels to transmit the virus.
The most common ways hepatitis B is spread include:
- sexual contact
- sharing of injecting equipment
- needlestick injuries in a health care setting
- reuse of unsterilised or inadequately sterilised needles
- child-to-child transmission through contact such as biting
- sharing personal items such as razors, toothbrushes, or hair and nail clippers
- mother-to-baby, though it is to be noted that the Australian vaccination program has significantly reduced this risk through the administration of the vaccine within 12 hours of birth.
Hepatitis B is NOT spread by contaminated food or water, and cannot be spread through casual or social contact such as kissing, sneezing or coughing, hugging, or eating food prepared by a person with hepatitis B.